Childhood continence
Dr Ba’Ath has special interest in continence in children, whether for urine or stool. He passionately believes that every child deserves to be socially clean if they wish, regardless of their mental ability and disease process. Dr Ba’Ath currently chairs the Syrian Children’s Continence Interest Group (SCCIG). This is a group of physicians inside and outside Syria, mostly of Syrian decent that concerns itself with these common, but often undertreated problem. The group produced locally tailored guidelines, suitable to the Syrian context and have introduced treatments to the region that were not used before, such as the bed alarms.
Day time wetting
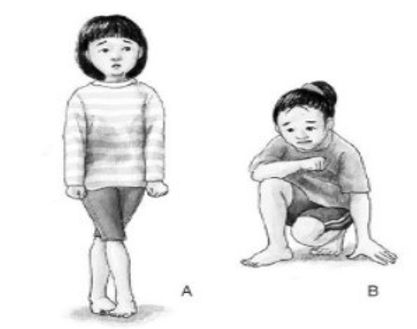
A very common problem in children, especially school age children, particularly girls. Most of it is in the category of urge incontinence. This usually presents as dribbling urine and spotting of the underwear during the day, often associated with sudden, severe urge to void that gives the child little warning to get to the toilet. It might be associated with certain body postures and maneuvers such as the one shown in the picture below. These maneuvers are attempts by the child to block the flow of urine to stop the wetting. In the one on the right, known as “Vincent Courtesy Sign”, the heel is pressing against the urethra. The one on the left, female children usually try to block urine flow by crossing the legs.
Most of these problems can be rectified by changing voiding habits and re-training the bladder to become less irritable. Again, close follow-up is required for successful treatment. This is a process known as “urotherapy”. Because it is essentially like acquiring a new habit, results take time to materialize. This usually means weeks. It is important not to expect a very quick fix.
The first step in training the bladder to contain urine is to make urine! Many kids suffering from wetting will stop or reduce fluid intake to prevent accidents from happening. This is a mistake and can have detrimental effects on health. In Dubai’s weather, children should drink 1200 to 1500 milliliters in a day. This can be juice, water, or milk. Caffeine containing drinks, like energy drinks, tea and coffee should be avoided.
The next step in urotherapy is to train the bladder to hold on to the urine. This is usually done by asking the child to respond to the first voiding sensation by trying to make it go away. Often this is successful. In clinic, I usually demonstrate to the child that the bladder is not full by using the ultrasound despite their sensation of the need to void. This form of objective biofeedback often enables the child to regulate and control his sensation. A normal bladder will be completely silent when it is less than half full.
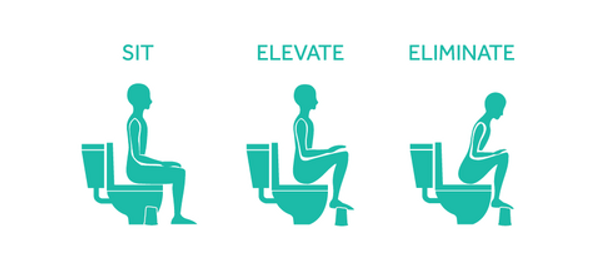
The last step in urotherapy is timed and complete voiding. I usually ask the child to make a trip to the bathroom every 3 hours of wake time, regardless of the sensation to void and including school hours. When the child goes to the toilet, they need to urinate while sitting down (even boys). Toilet access in public and schools might be an issue for some children. While on the toilet, the legs should be slightly elevated and the child should bend forward slightly, as shown in the picture below, in a “sit, elevate, eliminate” sequence. A small step or platform might be useful. Girls should sit with their knees apart, to avoid urine refluxing back into the vagina and then dribbling when they stand up, which is known as “vaginal voiding”.
Children should be deliberate about emptying their bladder completely and given enough time on the toilet to achieve that. This usually means a few minutes. Sometimes “double voiding” is required, i.e., a first void, followed by 10 minutes of walking, then another void. I usually make sure that the child has at least 1 successful attempt at emptying the bladder in clinic, confirmed with ultrasound, to set the standards for the family in terms of what to do to empty the bladder completely.
Whistling or blowing gently (like blowing a feather) while urinating can help relax the pelvic floor and allow effective emptying of the bladder. Also for younger children it might help to make the whole thing like a game by asking the child to make a continuous “whoooosh” sound of the urine falling into the toilet rather than an interrupted “sh.. sh .. sh”.
Day time wetting
Bed wetting
A very common problem in children. Up to 15% can be affected. Not normal after the age of 5 and should be treated to avoid long term psychosocial effects. Very occasionally it might indicate a serious medical problem, hence seeking medical attention is necessary. Most of the time treatment can be simple by following appropriate advice, bed wetting alarm, or medication. Appropriate treatment requires close follow-up by the treating physician. Dr Ba’Ath would normally offer direct access to patients to facilitate the care of children with continence problems.
Dr Ba’Ath produced this promotional video regarding bed wetting.
Bed wetting alarm is an internationally recognized method for treatment of bed wetting. These devices are available commercially. Dr Ba’Ath produced these two videos about two commonly used ones.
Neurogenic Bladder
The bladder is somewhat a unique organ in that it has combined voluntary and involuntary control. This keeps the kidney safe by maintaining urine storage under low pressure while at the same time giving us the ability to be socially continent, so we don’t wet ourselves or void when it is not appropriate. When the nerves of the bladder are not normal, these functions are disrupted. This is commonly associated with problems of the spine.
These children usually require plenty of medical input and multi-disciplinary care. The focus in the first few years of life is to keep the kidneys safe and keep the child infection free as much as possible. Later, and when the child desires, achieving social continence becomes another treatment goal.
Treatment is a very large topic and some parts of it are controversial, even amongst practicing clinicians. Most children will need to empty their bladder artificially through a process called clean intermittent catheterization. Occasionally minor or major surgery might be needed. These patients often have long-term relationships with their medical carers and become sort of friends, which helps in getting the best outcome.
Day time wetting
Fecal Incontinence
A very common and often undertreated problem in children with significant psychosocial effects. Generally divided into two types: pseudoincontinence (false incontinence) and real incontinence. The pseudoincontinence results from severe constipation leading to overflow diarrhea. Sometimes treatment is difficult and requires perseverance and very close follow up. Also, sometimes it is associated with neurogenic bladder, and in such circumstances, children will have neurogenic bowel as well, because the bladder and the bowel share nerve supply. As Dr Ba’Ath is double qualified to deal with general surgical and urological problems, he is best suited to care for this group of children.
Constipation
A very common problem in modern pediatric practice. In some studies, up to 30% of all children are affected. It can be easily missed and neglected or undertreated. Most constipated children can be cared for by the general pediatrician or the pediatric gastroenterologist. Occasionally, surgical input is required. Signs that surgical input is needed include severe, early onset constipation, failure of medical therapy, presence of abdominal distension, explosive motions, association with vomiting or poor growth, and stool shaped like thin toothpaste. Dr Ba’Ath made this educational video about when constipation becomes a surgical problem.